Science
Microbiome 101: Nurture Your Microbiome for a Healthier You
As you age, paying attention to your gut health becomes increasingly important. Environmental factors, stress & diet can each impact your gut health and weaken your body’s natural defenses. By understanding the role of your microbiome, SCFAs, fiber, and the gut-brain axis, you can take proactive steps to support your digestive, mental and overall health. Start by incorporating fiber into your diet, managing stress, get moving and staying hydrated to keep your microbiome thriving. Your gut—and your body—will thank you!
Understanding Your Microbiome:
A Guide for Healthy Aging
What is the Microbiome?
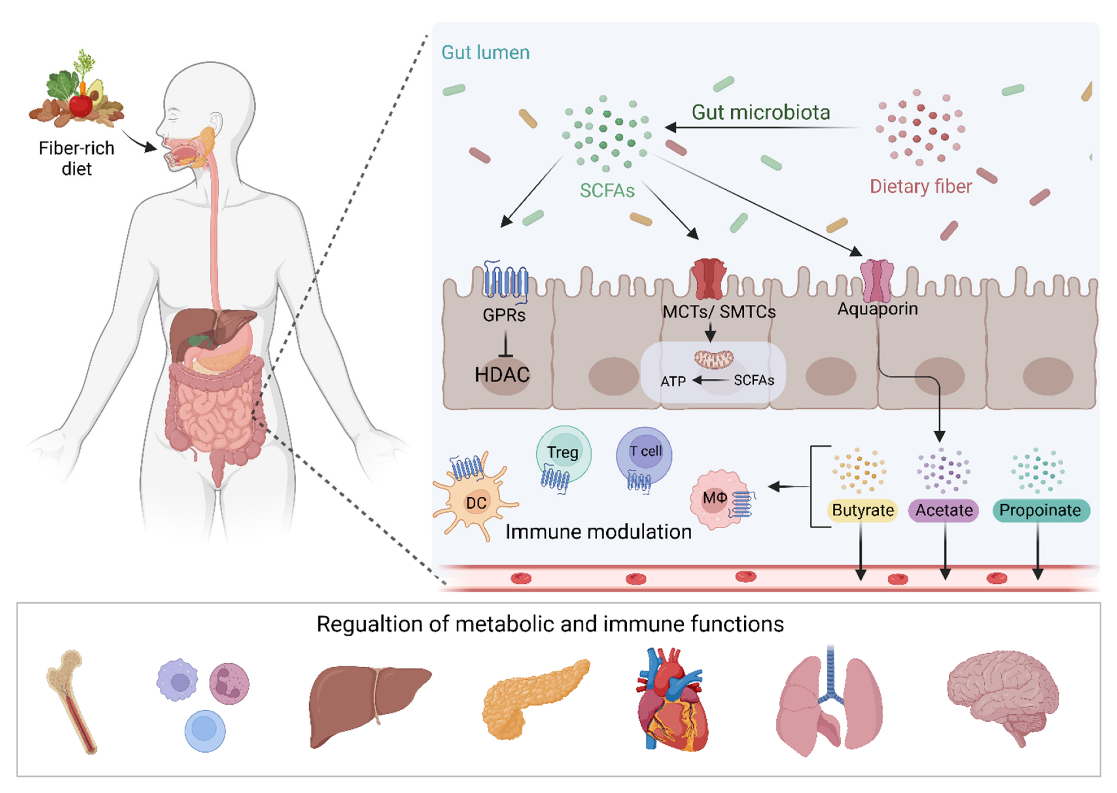
Your microbiome is a vast community of trillions of microbes, including bacteria, viruses, and fungi, that live in your gut. These microbes play a crucial role in your overall health, from supporting your immune system to helping digest food and even influencing your mood. A balanced microbiome is essential for maintaining good health as you age, as it helps protect against harmful pathogens, supports the production of vital nutrients and keeps your digestive tract working properly. [1][2].
Healthy microbiome = balanced microbiome –more beneficial SCFA producing bacteria & less harmful bacteria
Dysbiosis = unbalanced microbiome – leading to improper gut cellular functions
Leaky gut = increased intestinal permeability allowing harmful toxins into the bloodstream
Leaky Gut Syndrome
The Role of Fiber
Fiber is a type of carbohydrate that your body can’t digest, but your gut bacteria can. It acts as fuel for your microbiome, promoting the growth of beneficial bacteria and the production of SCFAs. Fiber also helps regulate bowel movements, prevents constipation, and supports a healthy gut environment by keeping harmful bacteria in check. Aim for a diet rich in fruits, vegetables, whole grains, and legumes to ensure you’re getting enough fiber[5][6].
Click the link below to learn how to incorporate more fiber into your diet.
What Are SCFAs?
Short-chain fatty acids (SCFAs) are compounds produced when gut bacteria (in your microbiome) break down dietary fiber. The three main SCFAs are acetate, propionate, and butyrate, which are vital for gut health. They provide energy to the cells lining your colon, help maintain the gut barrier and reduce inflammation. SCFAs have also been linked to improved immune function and may help prevent chronic diseases like certain cancers and bowel disorders[3][4].
Butyrate is the most researched and highly regarded because of its functionality. According to Xiong R-G, et al (2022), Butyrate exerts multiple effects such as preventing and inhibiting colon cancer, improving intestinal inflammation, and regulating intestinal pain thresholds and motility.
A diet high in fiber can help promote the production of SCFAs and contribute to a healthy gut microbiome.
The Gut-Brain Axis
The gut-brain axis is a complex communication network that links your gut and brain. Your gut microbiome plays a key role in this connection, influencing your mood, stress levels, and even cognitive function. For example, certain gut bacteria produce neurotransmitters like serotonin, which affects your mental health. A healthy microbiome can help maintain this balance, supporting both your digestive and mental well-being[7].
The gut-brain connection, commonly referred to as the gut-brain axis, is the studied bidirectional communication between the central and the enteric nervous system. The central nervous system (CNS) being the brain and spinal cord and the enteric nervous system (ENS) is the intrinsic nervous system that controls the GI tract. The ENS that regulates our gut is often called the body's “second brain.” Although it can't compose poetry or solve chemical equations, this extensive & complex network uses the same chemicals and cells as the brain to help us digest and to alert the brain when something is amiss.
This gut/brain connection links the emotional and cognitive centers of the brain with gastetointestinal tract. Recent studies have described the importance of the gut microbiota in influencing these interactions.
Microbiome & Constipation
Constipation is often linked to an imbalance in the gut microbiome. When your diet lacks sufficient fiber, your gut bacteria produce fewer SCFAs, which are essential for maintaining healthy bowel movements. Over time, without proper fiber food, the SCFA producing bacteria go away and are overrun by pathogenic bacteria.
Additionally, the brain can influence gut motility. Stress or anxiety may also contribute to constipation through the complex microbiome and the nerve cells in the gut linked to the vagus nerve that travels to and from the brain.
In Parkinson’s, the loss of dopamine-producing neurons in the brain also affects the gut. This dopamine deficiency can disrupt the contraction of muscles in the intestines, leading to slowed gastric motility and constipation.
By eating a fiber-rich diet and supporting a balanced microbiome, you can improve gut health and reduce the risk of constipation[8].
https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.999001/full
https://www.gutmicrobiotaforhealth.com/why-short-chain-fatty-acids-are-important-for-a-healthy-gut/
https://www.medicalnewstoday.com/articles/short-term-increase-in-fiber-alters-gut-microbiome
https://www.everydayhealth.com/digestive-health/experts-why-is-fiber-important.aspx
NeuroFiber Data
Sorridi Therapeutics conducted two studies to assess the health promoting potential of NeuroFiber Prebiotic Bars.
NeuroFiber: Ex-Vivo Study
As it is well documented that PD patients have reduced SCFA production, one of NeuroFIber’s goals is to increase SCFA production to facilitate a healthier gut lining. Using Cryptobiotix’s ex-vivo SIFR® technology, Sorridi Therapeutics studied the impact of NeuroFiber prebiotic bars on metabolite production (key fermentative parameters - gas, pH, and SCFA’s) of the gut microbiota of People with Parkinson’s.
NeuroFiber Dark Chocolate Cherry was tested against the market leading stool softener, propylene glycol and a No Substrate Control (NSC).
Results show that NeuroFiber Chocolate Cherry significantly decreased pH, key to fighting off pathogenic bacteria, and greatly stimulated the production of total SCFA’s (acetate, propionate, butyrate).
Total Scfa Production (mM)
Key takeaways
NeuroFiber Bar had a significantly higher amount of SCFA production vs. control and it does this while producing less gas than the market leading fiber bar. The lower the gas/SCFA ratio, the better, making it more tolerable than other fiber bars. The current market leading stool softener matches the control, producing zero increase in SCFA production.
*Data Shows Significant Results From 6 Participants In Ex Vivo Trial Conducted Using Cryptobiotix SIFR Technology. Key fermentation parameters were assessed at 24h after introduction of test products in colonic environment of human adults, as simulated with the Ex Vivo SIFR® Technology. Six test subjects were included in the study design, thus ensuring representative findings.
Sorridi Therapeutics conducted a one-month, open label pilot clinical trial with NeuroFiber Bars in People with Parkinson’s.
Objective
The study objective was to characterize and evaluate changes in gut-inflammation, gut-derived bile acids and SCFAs, and disease management parameters in adults with Parkinson’s disease before and after 4-week intake of 1/day NeuroFiber®, a novel prebiotic fiber bar.
Preliminary results showed:
Significant shifts in gut-derived metabolite pools of bile acids
A decreasing trend in gut inflammation as measured by Calprotectin
Significant reductions in Total Cholesterol, LDL-cholesterol and Non-HDL cholesterol, which is a great indicator of metabolic health.
Though not statistically significantly, SCFA’s did increase after 4 weeks and NfL and GFAP (neuroinflammation biomarkers) showed a favorable trend downwards. Significance is expected with a larger clinical trial.
Participant feedback on quality of life, QoL, measures were outstanding.
Survey results demonstrated improvements in sleep, bowel regularity, and most participants reported improvement in non-motor and motor experiences of daily living.
66.7% of study participants self-reported improvements in sleep (PDSS-2)
86.6% of study participants self-reported improvements in non-motor and motor experiences of daily living
Great improvements in GI Symptoms:
75% of those who reported mild to severe constipation at study initiation felt an improvement at the time of completion
40% of study participants saw an improvement in bowel movement straining
46.6% of study participants saw a reduction in hard or lumpy stools
25% of study participants reduced their laxative consumption during the trial